Experiencing sudden, intense facial pain can be alarming and disruptive to daily life, often leaving individuals seeking answers and relief. Trigeminal neuralgia is a chronic condition that affects the trigeminal nerve, responsible for transmitting sensations from the face to the brain. This condition is characterized by sharp, electric-shock-like pain, typically triggered by routine activities such as eating, talking, or even a gentle breeze.
Understanding the underlying causes, recognizing the symptoms, and exploring effective management strategies are crucial steps in alleviating the distress associated with this condition. This guide aims to provide a comprehensive overview of trigeminal neuralgia, offering valuable insights into its complexities and highlighting pathways to manage and potentially improve quality of life for those affected.
Overview of Trigeminal Neuralgia
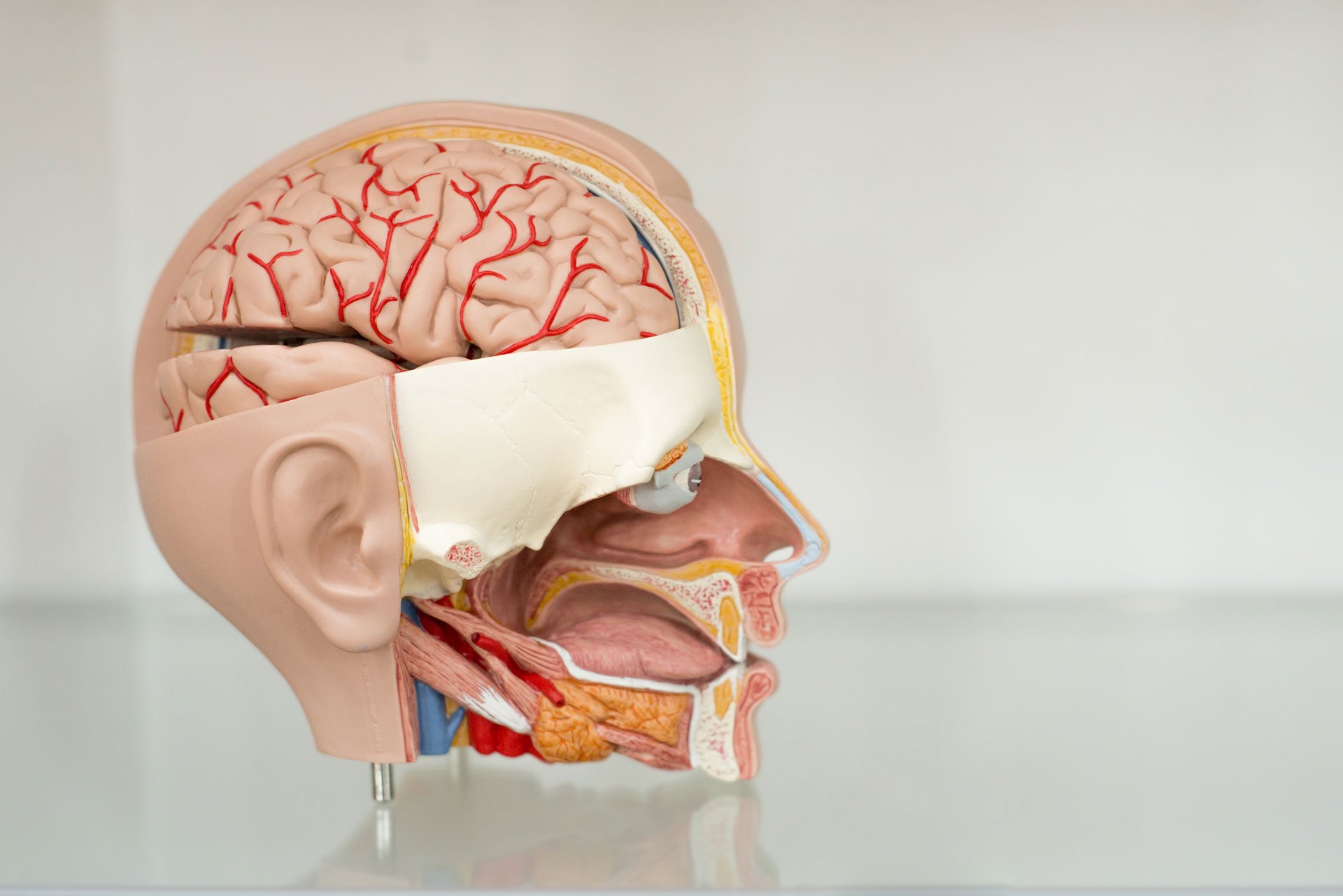
Trigeminal neuralgia (TN) is a chronic pain condition known for its sudden, intense facial pain episodes. This debilitating condition affects the trigeminal nerve, which is responsible for transmitting sensory information from the face to the brain. The trigeminal nerve, the fifth cranial nerve, comprises three branches: ophthalmic, maxillary, and mandibular. Each plays a crucial role in facial sensation, relaying signals like touch, pain, and temperature to the brain.
In individuals with TN, this nerve becomes hyperactive or damaged, often due to compression by blood vessels, leading to sharp, electric-shock-like pain in one or more branches. These painful episodes can last from seconds to minutes, severely impacting a person’s daily life. Activities such as eating, speaking, or exposure to a light breeze can trigger these attacks, making routine tasks daunting and stressful.
The unpredictability and severity of TN pain can lead to significant emotional and psychological distress, often resulting in anxiety and depression. The impact on quality of life is profound, as individuals may avoid social interactions and activities that could trigger an attack. Understanding TN’s cause and mechanisms is essential for effective management and treatment, aiming to reduce the frequency and intensity of pain episodes and improve the overall well-being of those affected. Comprehensive treatment strategies can include medication, surgical options, and lifestyle modifications, tailored to each patient’s needs.
Related: Expert Tips for Managing Parkinson’s Disease in Lutz, Florida
Causes of Trigeminal Neuralgia

Trigeminal neuralgia (TN) is primarily caused by factors that affect the trigeminal nerve’s structure and function, leading to severe facial pain episodes. Key causes include:
- Arterial Compression: The most common cause of TN is the compression of the trigeminal nerve by an artery. This pressure leads to damage and irritation of the nerve fibers, triggering painful episodes. Microvascular decompression surgery often relieves symptoms by alleviating this pressure.
- Demyelination: The protective myelin sheath surrounding the trigeminal nerve fibers can become damaged due to various reasons, including multiple sclerosis. This demyelination disrupts normal nerve signaling and can lead to the spontaneous generation of pain signals.
- Venous Compression: Although less common, compression by veins may also contribute to the condition. However, its significance is debated, and it is often not a primary focus during surgical interventions.
- Space-occupying Lesions: Tumors or cysts in the posterior fossa can exert pressure on the trigeminal nerve, leading to neuralgia. These conditions require careful diagnosis and management.
- Arachnoid Adhesions: These fibrous bands can bind nerve structures and contribute to nerve compression, though they are less frequently implicated compared to arterial compression.
Understanding these causes is crucial for accurate diagnosis and effective treatment of TN. Management strategies may vary depending on the underlying cause, ranging from medication to surgical intervention, aimed at reducing pain and improving quality of life for those affected by this debilitating condition.
Related: Carotid Artery Occlusion: Causes, Symptoms, and Treatment Approaches
Recognizing the Symptoms
Trigeminal neuralgia (TN) is characterized by distinct symptoms that can significantly impact an individual’s quality of life. Recognizing these symptoms is crucial for proper diagnosis and management. Key symptoms include:
- Electric Shock-like Pain: TN is marked by sudden, intense episodes of facial pain resembling electric shocks. These episodes are usually unilateral, affecting one side of the face, and can last from a few seconds to several minutes.
- Pain Location: The pain typically affects one or more branches of the trigeminal nerve, commonly the maxillary or mandibular branches. It can be mistaken for dental issues due to its localization in the jaw and cheek areas.
- Trigger Sensitivity: Pain attacks are often triggered by light stimulation, such as touching the face, chewing, speaking, or even exposure to wind. This hypersensitivity can make everyday activities challenging.
- Frequency and Patterns: Patients may experience multiple attacks per day, and the frequency can increase over time. The unpredictability of attacks adds to the distress, often leading to anxiety about when the next episode might occur.
- Associated Symptoms: Continuous aching pain can accompany the paroxysmal attacks, a condition known as atypical trigeminal neuralgia. This can complicate diagnosis and treatment as it may not respond well to conventional therapies.
Understanding these symptoms helps in early detection and intervention, improving outcomes for those affected by TN. Accurate recognition of pain patterns and triggers is essential for tailoring effective treatment plans, which may include medication, lifestyle adjustments, or surgical options.
Related: Hemicrania Continua: Rare Chronic Headache Disorder Overview
Diagnosing Trigeminal Neuralgia

Diagnosing trigeminal neuralgia (TN) involves a comprehensive evaluation to differentiate it from other facial pain disorders. Accurate diagnosis is crucial for effective treatment. Here are key aspects of the diagnostic process:
- Symptom Assessment: Diagnosis begins with a detailed patient history to identify characteristic symptoms. TN typically presents as sudden, severe, unilateral, electric shock-like facial pain triggered by touch or movement.
- Clinical Criteria: Diagnosis is based on meeting specific criteria, including the paroxysmal nature of pain and its distribution along the trigeminal nerve branches. Pain should not extend beyond the trigeminal territory.
- Types of TN: Differentiation between classical, secondary, and idiopathic TN is essential. Classical TN is often linked to vascular compression, while secondary TN results from underlying neurological diseases like multiple sclerosis.
- Imaging Tests: Magnetic resonance imaging (MRI) is used to identify structural causes, such as neurovascular compression or lesions. MRI can help distinguish classical TN from secondary forms.
- Neurophysiological Tests: Trigeminal reflex testing may be performed to assess nerve function, particularly in atypical cases or when MRI is inconclusive.
- Diagnostic Challenges: TN diagnosis can be challenging due to the overlap with other conditions like dental issues or atypical facial pain. Misdiagnosis may lead to unnecessary treatments.
Early and accurate diagnosis of TN is crucial for initiating appropriate interventions, reducing pain episodes, and improving patients’ quality of life. Tailoring the diagnostic approach to individual symptoms and leveraging advanced imaging techniques can enhance diagnostic accuracy.
Related: Multiple Sclerosis (MS): Understanding the Disease and Treatment Strategies
Management and Treatment Strategies
Managing trigeminal neuralgia (TN) involves a multimodal approach to alleviate the intense facial pain and improve quality of life. Effective management strategies include:
- Medication: First-line treatments typically involve anticonvulsants such as carbamazepine and oxcarbazepine, which help reduce nerve pain by stabilizing nerve activity. Tricyclic antidepressants may also be prescribed to manage chronic pain.
- Surgery: For individuals who do not respond to medication, surgical options are available. Microvascular decompression is a preferred method, offering long-term relief by alleviating pressure on the trigeminal nerve. Other surgical interventions include rhizotomy and Gamma Knife radiosurgery, which target nerve fibers to block pain signals.
- Emerging Therapies: Advances in treatment include neuromodulation techniques like deep brain and motor cortex stimulation, offering relief for patients refractory to traditional methods. These therapies show promise but require further study to confirm their efficacy and safety.
For those in Lutz, Florida, seeking expert care, consider visiting the Center for Neurology. Dr. Kavita Kalidas, a board-certified neurologist and UCNS-certified headache specialist, provides comprehensive care tailored to each patient’s needs. Her expertise ensures that patients receive the most current and effective treatment strategies for managing trigeminal neuralgia.
These diverse treatment options underscore the importance of a tailored approach to managing TN, focusing on patient-specific factors to optimize outcomes and enhance quality of life.