Understanding carotid artery occlusion is crucial for anyone facing this condition, as it can significantly impact cardiovascular health. This medical issue involves the narrowing or blockage of the carotid arteries, which are vital pathways supplying blood to the brain. Recognizing the causes and symptoms is essential for early detection and management, thereby reducing the risk of serious complications such as stroke.
Fortunately, with advances in medical treatments and intervention strategies, there are effective ways to address carotid artery occlusion. By exploring the underlying factors, identifying warning signs, and discussing diverse treatment approaches, individuals can be better prepared to manage this condition and improve their quality of life.
What is Carotid Artery Occlusion
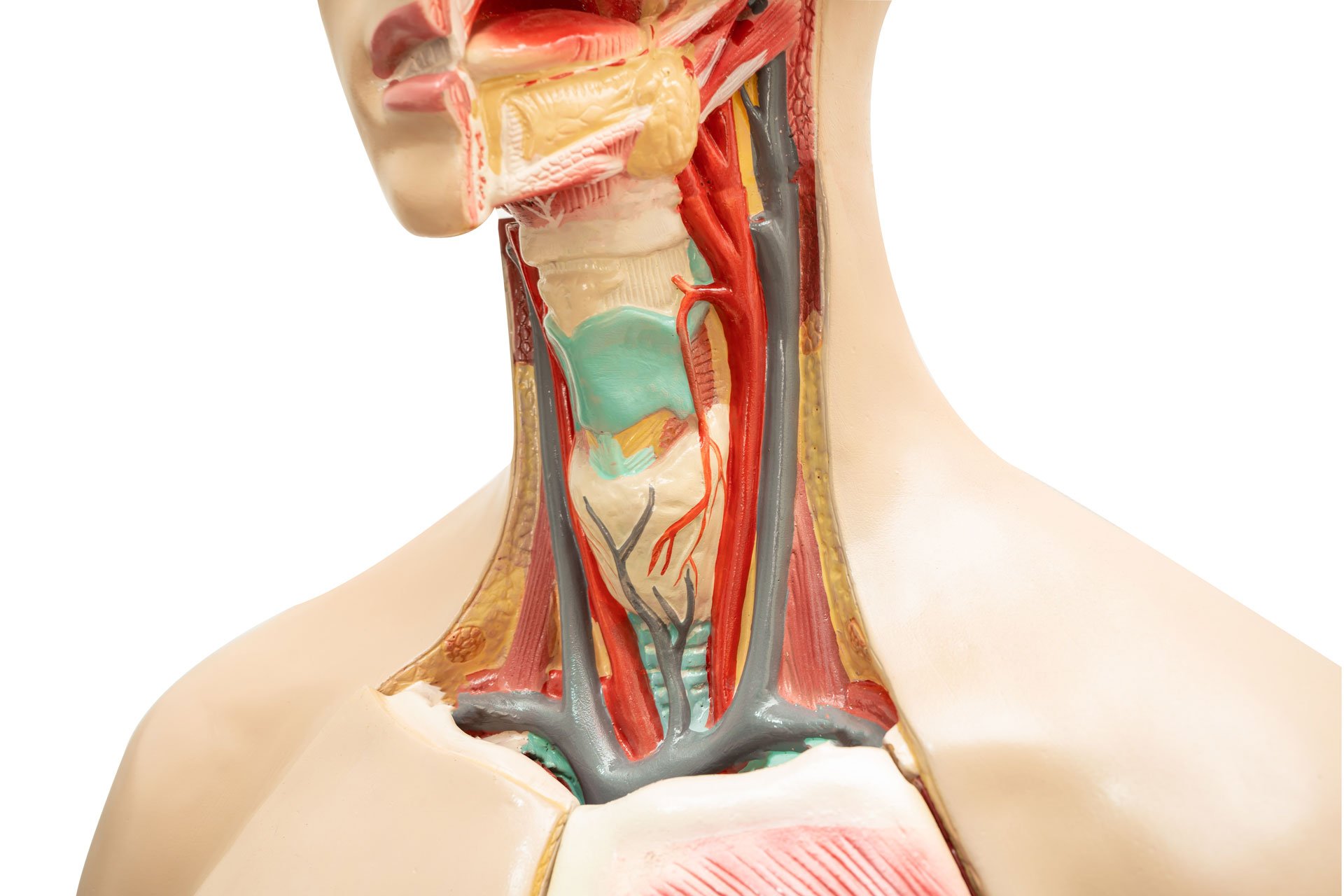
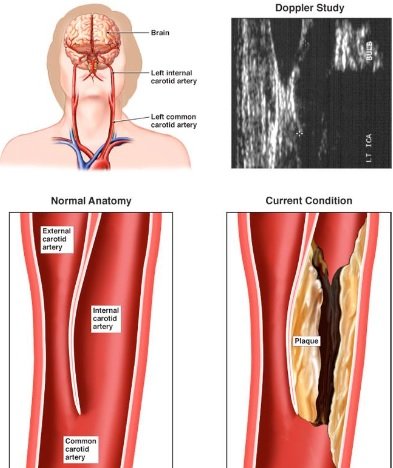
Carotid artery occlusion is a condition where the carotid arteries, major blood vessels located on each side of the neck, become narrowed or blocked, primarily due to atherosclerosis. Atherosclerosis is the buildup of fatty deposits, known as plaques, which consist of cholesterol, fats, and other substances found in the blood.
These plaques can thicken and harden, leading to the narrowing (stenosis) or complete blockage (occlusion) of the artery, disrupting the critical blood flow to the brain. This disruption significantly increases the risk of stroke, which can result in severe neurological damage or even death.
The progression of carotid artery occlusion is often gradual and might not present noticeable symptoms until it becomes severe. The primary risk factors include high blood pressure, diabetes, smoking, high cholesterol, and a sedentary lifestyle. As part of the circulatory system, the carotid arteries are vital for transporting oxygen-rich blood to the brain.
Thus, maintaining their health is crucial for overall cerebral function. Regular monitoring and management of risk factors are essential to prevent the development or progression of this condition, thereby reducing the likelihood of future strokes and improving long-term health outcomes.
Related: Hemicrania Continua: Rare Chronic Headache Disorder Overview
Causes of Carotid Artery Occlusion
Carotid artery occlusion occurs when the carotid arteries, critical vessels supplying blood to the brain, become narrowed or blocked. This condition is primarily caused by the buildup of atherosclerotic plaque. Understanding the underlying causes and risk factors is essential for managing and preventing this condition. Here are the main causes and risk factors:
- Atherosclerosis: The most common cause, where fatty deposits or plaques accumulate on the artery walls, leading to narrowing and potential blockage.
- High Blood Pressure: Increased pressure on arterial walls can accelerate plaque buildup and damage the arteries.
- High Cholesterol: Elevated levels of LDL cholesterol contribute to plaque formation and arterial narrowing.
- Diabetes: This condition affects the body’s ability to process fats, increasing the risk of atherosclerosis and subsequent occlusion.
- Smoking: Tobacco use damages blood vessels and accelerates the development of atherosclerosis.
- Obesity: Excess weight can lead to hypertension and increased cholesterol levels, further promoting plaque buildup.
- Sedentary Lifestyle: Lack of physical activity is associated with higher cholesterol levels and weight gain, both risk factors for artery occlusion.
- Family History: A genetic predisposition to cardiovascular diseases can increase individual risk.
Addressing these risk factors through lifestyle changes and medical intervention can help mitigate the risk of carotid artery occlusion and its severe complications, such as stroke.
Related: Multiple Sclerosis (MS): Understanding the Disease and Treatment Strategies
Recognizing Symptoms
Recognizing the symptoms of carotid artery occlusion is vital for early intervention and prevention of severe complications such as stroke. Often, carotid artery disease may not present noticeable symptoms until a transient ischemic attack (TIA) or stroke occurs, making awareness crucial. Here are the primary symptoms to watch for:
- Sudden Numbness or Weakness: Particularly on one side of the body, affecting the face, arm, or leg.
- Sudden Trouble Speaking: Difficulty in forming words, slurred speech, or an inability to understand speech.
- Vision Disturbances: Blurred vision or sudden loss of vision in one or both eyes.
- Dizziness or Loss of Balance: Unexpected dizziness, difficulty walking, or coordination issues.
- Severe Headache: A sudden and severe headache with no known cause.
- Confusion or Trouble Understanding: Sudden onset of confusion or trouble comprehending simple instructions.
A transient ischemic attack, often termed a “mini-stroke,” may present these symptoms temporarily. They serve as a critical warning sign of a potential full stroke. If you or someone you know experiences any of these symptoms, seek emergency medical assistance immediately. Early detection and treatment are essential to reducing the risk of a major stroke and ensuring better long-term health outcomes. Regular check-ups and monitoring are also advised for those with risk factors for carotid artery disease.
Related: Finding a Headache Doctor in Lutz, Florida: Top Tips
Diagnostic Techniques
Accurate diagnosis of carotid artery occlusion is crucial for effective treatment and prevention of strokes. Several diagnostic techniques are commonly used to evaluate the presence and severity of blockage in the carotid arteries:
- Carotid Ultrasound: This non-invasive test uses sound waves to create real-time images of the carotid arteries. It can detect areas with restricted blood flow due to narrowing or blockage.
- Computed Tomography Angiography (CTA): CTA employs X-rays to produce detailed images of the carotid arteries. A contrast dye is injected into the bloodstream to highlight the arteries and identify any blockages.
- Magnetic Resonance Angiography (MRA): Similar to CTA, this technique uses magnetic fields and radio waves instead of X-rays to generate images, providing a detailed view of the carotid arteries without radiation exposure.
- Cerebral Angiography: This minimally invasive procedure involves threading a catheter through the blood vessels to the carotid arteries. A contrast dye is injected, and X-rays are taken to visualize blood flow and pinpoint blockages.
These diagnostic methods are selected based on individual patient needs and can help healthcare providers determine the best course of action, whether it’s monitoring or proceeding with an intervention to restore blood flow and reduce stroke risk. Regular screenings and early detection are vital for individuals with risk factors for carotid artery occlusion.
Related: Transient Ischemic Attack (TIA): Warning Signs and Preventive Measures
Potential Complications
Carotid artery occlusion can lead to serious health issues if not addressed promptly. Understanding the potential complications is essential for those affected by this condition. Here are the primary complications associated with carotid artery occlusion:
- Stroke: The most significant risk of carotid artery occlusion is the development of a stroke. When blood flow to the brain is severely reduced or blocked, it can result in permanent damage or death of brain cells, leading to severe disability or even fatality.
- Transient Ischemic Attack (TIA): Often referred to as a “mini-stroke,” a TIA is a temporary blockage that presents similar symptoms to a stroke but resolves within 24 hours. It serves as a critical warning sign for a potential major stroke.
- Cognitive Impairment: Repeated TIAs or a significant stroke can lead to cognitive decline, affecting memory, speech, and the ability to perform daily tasks.
- Paralysis: Depending on the stroke’s severity and location, paralysis on one side of the body can occur, impacting mobility and independence.
- Vision Problems: Occlusion can lead to sudden vision loss or blindness in one or both eyes, severely affecting quality of life.
- Speech Difficulties: Damage to specific brain areas can result in aphasia, a condition that impairs the ability to communicate effectively.
Early detection and management of carotid artery occlusion are crucial in mitigating these risks and improving patient outcomes. Regular monitoring and appropriate interventions can help prevent these serious complications.
Treatment Approaches
Treatment approaches for carotid artery occlusion focus on restoring adequate blood flow to the brain and minimizing the risk of stroke. Here are the primary treatment options available:
- Lifestyle Modifications: Patients are encouraged to quit smoking, adopt a heart-healthy diet, and engage in regular physical activity to manage cholesterol and blood pressure.
- Medications: Antiplatelet agents like aspirin, anticoagulants, and statins are prescribed to reduce the risk of blood clots and manage cholesterol levels.
- Carotid Endarterectomy: This surgical procedure involves removing plaque from the carotid artery to prevent future strokes. It is typically recommended for patients with significant artery narrowing.
- Carotid Angioplasty and Stenting: For patients unsuitable for surgery, this less invasive procedure involves using a balloon to widen the artery and placing a stent to keep it open.
For those seeking specialized care, the Center for Neurology in Lutz, Florida, offers comprehensive treatment options. Dr. Kavita Kalidas, a board-certified neurologist and UCNS-certified headache specialist, provides expert care tailored to individual needs. Early intervention and regular monitoring are critical steps in managing carotid artery occlusion and reducing associated health risks.